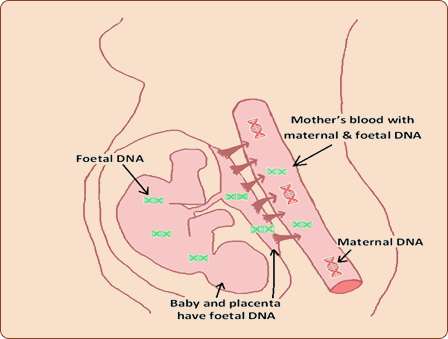
This is a new type of prenatal screening blood test that evaluates the likelihood of fetal trisomies by analysing cell- free DNA (cfDNA) in maternal blood. Circulating cell free fetal DNA is thought to be primarily derived from the placenta.
What are the common abnormalities detected on NIPT?
The most common chromosomal abnormalities seen in the general population are Trisomy 21(Down’s syndrome), Trisomy 18 (Edward’s syndrome) and Trisomy 13 (Patau’s Syndrome). NIPT can be used in pregnant women of any age or risk category to assess the likelihood of Trisomy 21, 18 and 13. It can also be used to detect sex chromosomal abnormalities of the fetus although that it has not been the primary target of prenatal screening.
How is the test done and what is the timing of the test?
Dating/ Viability scan is required prior to testing. Testing is usually offered by a single blood test draw from 10 weeks onwards as there may be insufficient DNA prior to this. The test can be applied to both in singleton and twin pregnancies resulting from natural conception or in vitro fertilisation (IVF). The median turn around time for the results is 10 calendar days.
What are the indications for testing?
NIPT is suitable for pregnant women at 10 weeks and above. However the most common indications for NIPT are
- a high risk combined first trimester screening result
- advanced maternal age
- a previous pregnancy with a fetal abnormality
- a previous history of chromosomal abnormality
- a family history of chromosomal abnormality
How is NIPT used in the clinical practice in Australia?
In Australia there are two patterns of implementation of this NIPT are identified. In the first, it is offered as a primary screening test at 10 weeks in conjuction with 12 weeks scan. In the second, NIPT is used as a secondary screen after a high risk result on combined first trimester screening test.
Who are the main providers of this test in WA?
NIPT became available in Australia in late 2012. Currently NIPT is accessed through four different overseas providers.
- Harmony (Ariosa, USA) – www.ariosadx.com
- Verify (Illumina, USA) – www.illumina.com
- Panorama (Natera, USA) – www.panoramatest.com
- iGene screen( BGI, China) – www.igenescreen.com
How accurate are the results?
NIPT represents the most accurate form of prenatal screening test for Down’s syndrome with a detection rate of 99% and a false positive rate of less than 0.5%. The detection rate is slightly less but impressive in fetuses with Trisomy 18 (detection rate of 97%) and Trisomy 13 (detection rate of 92%). Hence a negative cfDNA test result does not always ensure a chromosomally normal fetus. With a positive test result, confirmation of fetal karyotype with CVS or amniocentesis is recommended as false positive results can occur.
What are the advantages of NIPT?
- Convenient and safe
- No risk of miscarriage
- High detection rate
- High accuracy of test results
- Low invasive test rate(<1.5%)
- Early results and decision making
What are the disadvantages of NIPT?
- Expensive
- Still a screening test. An invasive test is needed to confirm positive results on NIPT
- Significant test failure rate ( 3%)
- False positive and false negative test reults
- Loss of other benefits of first trimester screening
( Eg: Low PAPP-A levels in predicting intrauterine growth restriction and preeclampsia) - Not applicable to general population on current cost
Does NIPT replace 12-14 weeks scan?
NIPT is not used to replace the 12- 14 weeks scan as it is still recommended to rule out early major structural abnormalities. Nuchal translucency (NT) measurement still remains in use to detect increased NT measurement that would indicate cardiac and other anomalies.
Does this test replace invasive testing such as CVS or amniocentesis?
The greater accuracy and low false positive rate of NIPT minimises the chance of further invasive diagnostic testing such as chorionic villus sampling (CVS) and amniocentesis. However cfDNA does not replace the accuracy and diagnostic precision of prenatal diagnosis with CVS or amniocentesis. If a fetal structural anomaly is identified on ultrasound examination, invasive testing is usually offered.
Is there anything else I need to know about the test?
Fetal DNA is heavily diluted with maternal cfDNA and on average represents approximately 10% of the total cfDNA in maternal blood. This fetal fraction is positively correlated with gestational age and negatively correlated with maternal weight, thus increasing the chance of ‘ no result’ or unreliable result in women with a high BMI. To obtain reliable results, the minimum fetal fraction required is 4%. A redraw repeat test becomes necessary in about 3% of patients and the test provider offers a repeat test at no extra cost. The overall ‘no result’ rate is < 1% after a second test. Data is now emerging that women who experience test failure due to very low fetal fractions may need to be considered as being at increased risk of chromosomal abnormalities.
Who should I see to discuss prior to choosing NIPT?
You can discuss this test either with your GP or Obstetrician.


